Pregnancy and Pneumothorax: What Does the Research Say?
20 Feb 2024
Pregnancy can be a nervous and exciting time. However, when you live with a health condition such as Birt-Hogg-Dubé Syndrome there can be an added worry of whether your pregnancy could be affected by health issues such as lung collapse (also known as pneumothorax). In BHD, 44 to 75% of patients experience at least one lung collapse. This can occur between ages of 20 to 50 years, the same years a biologically female person can experience pregnancy and birth.
Individual lung collapse risk is hard to identify as there is a lack of reliable clinical markers (medical signs which can indicate whether a person may experience a lung collapse). The frequency of lung collapse in pregnant BHD patients has not been calculated before.
Lung collapse in pregnancy is understandably a worry for the person who is pregnant. You may worry that a lung collapse could harm you or your unborn child. This study aimed to understand the frequency of spontaneous pneumothorax in pregnant BHD patients to help inform patients and care.
How did they do this?
108 patients attending the Munich BHD Syndrome outpatient clinic between 2005 and 2022 and their relatives were included in this study. Participants were from mainly multiplex families with a BHD diagnosis. Patients were allocated to three groups:
- Group 1: Female (biological sex) BHD patients who had experienced at least one pregnancy and birth.
- Group 2: Female (biological sex) family members who have the FCLN mutation but had not experienced pregnancy or birth.
- Group 3: Female (biological sex) family members without BHD and had experienced at least one pregnancy and birth.
All but one family who took part were of German descent or Eastern European with German roots (known as Volga Germans). The remaining family was English in origin. All participants gave consent for DNA testing and mutation screening of the FCLN gene.
The clinical and pedigree information from these patients were used to calculate whether there is a risk relationship between pregnancy and pneumothorax.
What did they find?
Participants were split into three groups. Calculations were done on all three groups’ health information to see if there was a link between pregnancy and increased risk of pneumothorax:
- Group 1: In the BHD and pregnancies group, there were 46 participants. Pregnancies were at the average age of 30 years old. Eight incidences of lung collapse occurred during pregnancy. Lung collapse occurred at the same rate in the first pregnancy as in later pregnancies. This means having more than one pregnancy did not increase the rate of lung collapse. The average age for first lung collapse was 30.2 years.
- Group 2: 18 female (biological sex) family members of Group 1, who have the FCLN mutation but have never experienced pregnancy. The average age for first lung collapse was 30.4 years, which is very similar to Group 1.
- Group 3: 25 female (biological sex) family members without BHD who had experienced pregnancy were included in this group. This was a second control group and used to demonstrate that lung collapse is a rare event in the general population. There were no incidences of lung collapse in this group.
How far can we apply these findings?
This was a small study which can mean the results cannot be widely applicable to the global BHD population. However, larger scale patient studies of similar methods would increase understanding of findings.
The number of people in each group in this study varied. The BHD patients with pregnancy group (Group 1) was twice the size of the control group (Group 3). This could affect the findings because more participants = more possible lung collapses reported. However, in larger size studies this would be controlled for.
There could have been miscarriages which were unreported for various reasons. However, this not unusual in pregnancy and birth data.
What did this study help to do?
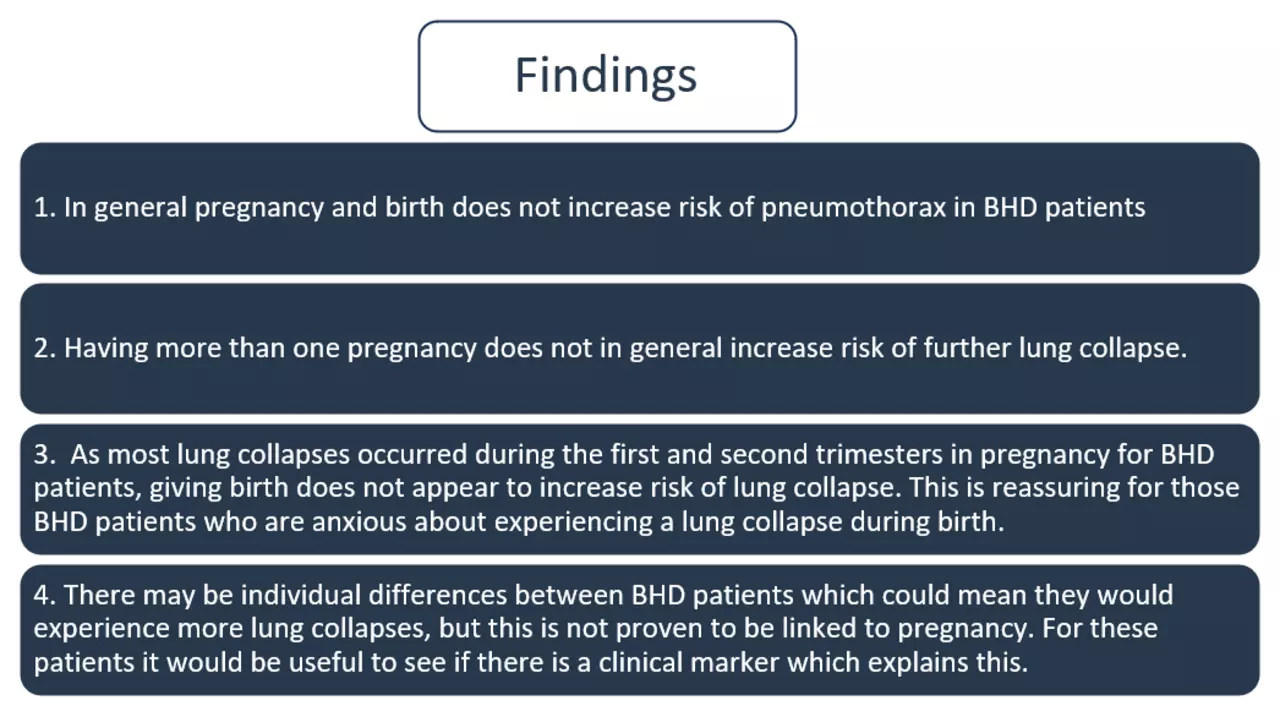
This study aimed to understand whether pregnancy increases risk of lung collapse in BHD patients. The findings indicate that pregnancy and birth do not increase risk of pneumothorax. However, this would need to be repeated on a much larger scale to be globally applicable. There could be some BHD patients who do experience repeated lung collapses after pregnancy, and it would be useful to know if there was a clinical marker that could predict this.
How does this affect me?
If you are a BHD patient and are pregnant, or are looking to become pregnant, it is important to be aware of the symptoms of lung collapse and to monitor these in case it does happen. This is the same advice given to all BHD patients. Symptoms such as shortness of breath, chest pain, and unusual coughing could indicate a lung collapse. It is also important that medical staff are trained to understand lung collapse symptoms in pregnancy so the right care can be given swiftly if this happens.
